AIoT in Healthcare: Real Cases, ROI, and a Pilot Playbook

Healthcare AIoT delivers when it lowers risk at the bedside and removes waste across the hospital. Think connected monitors, pumps, wearables, and imaging devices feeding models that spot deterioration early, triage alerts, and keep staff focused on care.
This article continues our series of articles about implementing AIoT across industries.
We’ll look closer at AI-powered IoT in healthcare: what to automate, where the model should run (edge, cloud, or hybrid), and how to prove value fast.
You’ll see where AIoT already works and how much it costs. We’ll walk through concrete case examples, map high-ROI use cases, and give you a KPI framework that balances clinical outcomes with operational metrics.
No fluff, no vendor pitch – just steps, numbers, and patterns you can apply from one of the top healthcare software development companies.
The Wave of Innovation – How AI-Powered IoT Looks in Healthcare
Case 1 – Mount Sinai (US): AIoT Early-Warning in ICU and Step-Down Care
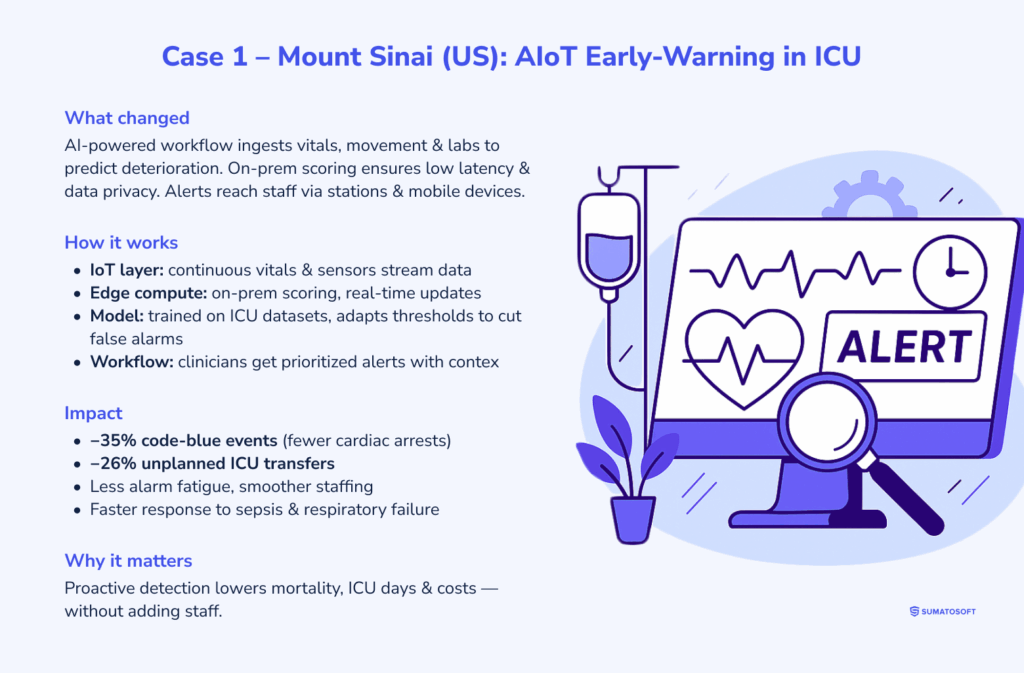
What changed: Mount Sinai Health System deployed an AI-powered early-warning workflow that ingests continuous bedside signals and recent labs to predict clinical deterioration. Inputs include ICU/step-down vitals (e.g., heart rate, respiratory rate, SpO₂), telemetry, movement, and near-real-time labs. These data streams flow from networked monitors and sensors into a hospital-hosted model for low-latency scoring. Alerts route to clinicians via central stations and mobile devices.
How it works (AIoT specifics):
- IoT layer – continuous vital-sign monitors and contact-free sensors stream patient data across the hospital network;
- edge/near-edge compute – scoring runs on-prem for latency and data residency; the model updates risk continuously rather than at fixed intervals;
- model behavior – trained on large ICU datasets, the model surfaces subtle trends (e.g., rising HR + declining SpO₂ + reduced movement) that precede crises; it adapts thresholds to reduce false alarms and focus attention on high-risk trajectories;
- clinical workflow – nurses and physicians receive prioritized alerts with enough context (signal pattern + recent labs) to trigger earlier assessments, orders, or transfers.
Impact (numbers):
- 35% fewer code-blue events – cardiac arrests requiring resuscitation after rollout, indicating earlier intervention and fewer nighttime emergencies;
- 26% fewer unplanned ICU transfers – reflecting earlier escalation from lower-acuity wards before patients crash;
- operational effects – fewer “all-hands” emergencies, lower alarm fatigue, and smoother staffing during high-acuity windows;
- clinical effects – faster response to sepsis and respiratory failure, and fewer prolonged ICU courses for some patients due to earlier stabilization.
Why it pays off: Code blues and unplanned ICU transfers carry high mortality, length-of-stay, and cost. Shifting from reactive to proactive care cuts adverse events, reduces high-intensity resource use, and improves outcomes without adding headcount.
Case 2 – Buckinghamshire NHS + MiiCare (UK): Smart-Home AIoT After Discharge
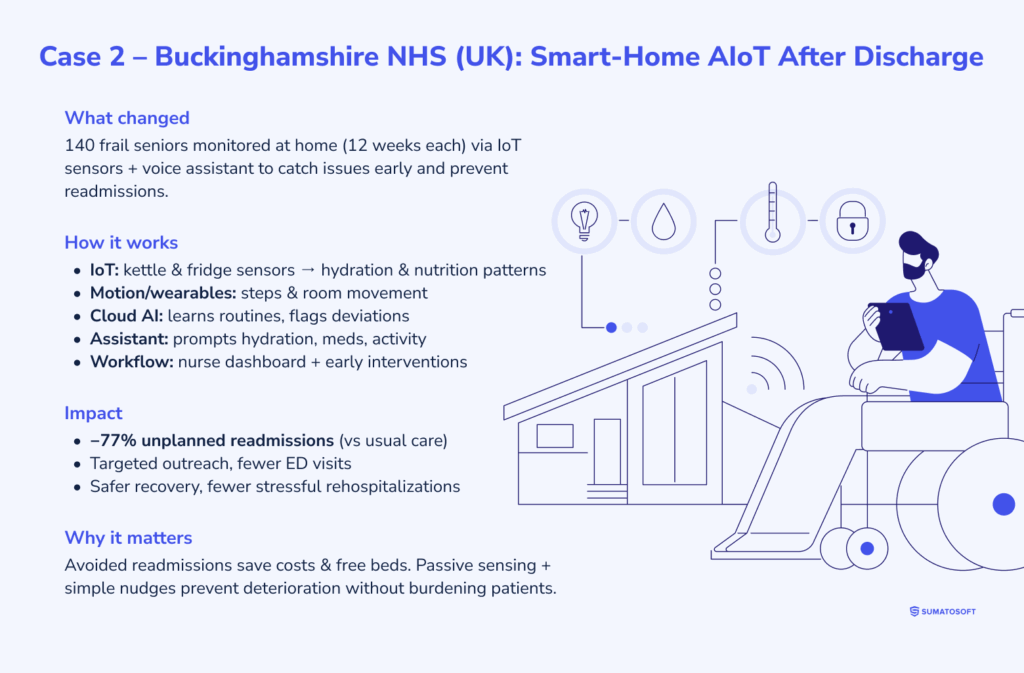
What changed: The “Onward Care” pilot monitored recently discharged frail seniors at home to catch problems before they led to readmission. Approximately 140 patients were enrolled for 12 weeks each. The program combined unobtrusive IoT sensors on everyday appliances with a virtual assistant to track routines and nudge activity.
How it works (AIoT specifics):
- IoT layer – small wireless sensors on kettles and refrigerators capture use patterns that proxy hydration and nutrition (e.g., morning kettle boils, fridge opens around meal times);
motion sensors and/or wearables add step counts and room-to-room movement; - cloud AI – a cloud model learns each person’s baseline routine and flags deviations (e.g., no kettle use all morning, sharp drop in steps, nighttime wandering);
alerts go to a nursing team via a dashboard; - in-home assistant – a voice device (“Monica”) prompts light activity, hydration, or medication adherence when inactivity or missed routines are detected;
- care workflow – when the AI flags risk, a nurse contacts the patient (call/visit) to intervene early – rehydration guidance, medication check, or GP escalation.
Impact (numbers):
- 77% reduction in unplanned readmissions – within six months versus usual care among high-risk elderly participants;
- scale signal – after the first year, the trust explored expanding the model to additional NHS sites based on outcomes and manageable workload;
- operational effects – more targeted outreach (fewer blanket check-ins), earlier course correction on dehydration/non-adherence, and fewer emergency department visits;
- patient effects – safer recovery at home, maintained routines, and fewer stressful returns to the hospital.
Why it pays off: Avoided readmissions save significant costs per case and free beds for higher-acuity admissions. Passive sensing avoids burdening patients; personalized baselines reduce false positives; and simple nudges (hydration, movement) often prevent a deterioration spiral.
What These Two Cases Show
- Different settings, same pattern: Whether in ICU (Mount Sinai) or post-discharge homes (Buckinghamshire), AIoT converts continuous signals into timely action, earlier escalation in hospital, and earlier outreach at home.
- Edge vs. cloud: Hospitals typically favor on-prem/near-edge scoring for latency and compliance; home programs lean on cloud AI for fleet-level learning and easy updates.
- ROI levers: The largest gains link directly to high-cost events: code blues, unplanned ICU transfers, and readmissions. Cutting these events compounds savings via shorter stays, fewer emergency interventions, and better bed availability.
- Human-in-the-loop: In both cases, AI augments- not replaces- clinicians. The lift comes from prioritized, trustworthy alerts and simple, actionable prompts that prevent drift into crisis.
Where AIoT Pays Off in U.S. Healthcare
There is a clear trend in healthcare AIoT: this technology links bedside monitors, wearables, and imaging machines to models that read vitals, waveforms, scans, and EHR notes in near real time.
The table summarizes where AIoT is used on the floor, the core methods behind it, the typical IoT impact on accuracy, speed, and cost, and named U.S. deployments that demonstrate these effects.
| Item | Description |
|---|---|
| AIoT usage | Medical devices that connect to the internet (wearables, smart monitors, imaging machines) gather patient information, which AI systems use to help doctors make diagnoses. AI algorithms process IoT sensor streams (vital signs from ICU monitors, ECGs, etc.) and medical images to identify early warning signs that clinicians might overlook. The system provides doctors with enhanced clinical decision support through ongoing data-based information. |
| AI methods | The main approach involves deep learning techniques (CNNs for medical image analysis of X-rays or MRIs) and supervised learning for pattern recognition in patient data. Time-series ML models analyze patient vital signs across time to forecast upcoming medical events such as sepsis onset and natural language processing (NLP) enables the analysis of electronic health records. The AI models achieve high accuracy in anomaly and disease indicator detection through training on extensive datasets containing medical outcome labels. |
| ROI impact | AI-assisted diagnostics can greatly improve accuracy and speed, leading to better outcomes and cost savings. Studies show AI can reduce diagnostic error rates by as much as 85%, which means fewer misdiagnoses and costly repeat tests. Faster, more accurate diagnoses also reduce unnecessary procedures and hospital days. In one U.S. hospital study, integrating an AI triage platform into radiology workflows delivered a 5-year ROI of ~451% (and up to 791% when accounting for physician time saved). Hospitals see financial returns through efficiency – for example, an AI system that automates scan analysis saved radiologists an estimated 145 work-days worth of time per year, allowing more patients to be served. |
| U.S. example | Mount Sinai Hospital (New York) deployed an AI-driven sepsis early-warning system that monitors patient vitals and lab results in real time. The AI (a machine-learning model on EHR and IoT monitor data) flags sepsis risk about 6 hours earlier than traditional methods, enabling earlier intervention. After implementation, Mount Sinai saw about a 20% reduction in sepsis mortality and shortened hospital stays for sepsis – a huge outcome improvement. Another example is a Texas hospital using an AI IoT platform for continuous sepsis monitoring, which reported 37% lower mortality and a 35% shorter ICU stay for at-risk patients. These cases highlight how AIoT diagnostics not only save lives but also provide tangible ROI by reducing critical care duration and associated costs. |
Building the Next Successful AIoT Case in Healthcare
This section turns AIoT from a promising idea into a pilot that ships. You’ll validate whether AI adds real lift beyond rules, spot early red flags, and run a one-week scan to surface a high-leverage use case.
We outline the minimal data you need (signals and outcomes), how to choose edge vs. cloud, and what to integrate with EHR and alerting so clinicians can act immediately.
This section helped you to:
- understand whether it’s a good idea to invest in AIoT;
- review the existing business and technical KPI of AIoT systems for healthcare;
- see a real-life example with cost calculations.
Is AI in IoT Right for You
A) Key Signs Your Healthcare IoT Will Benefit From AI
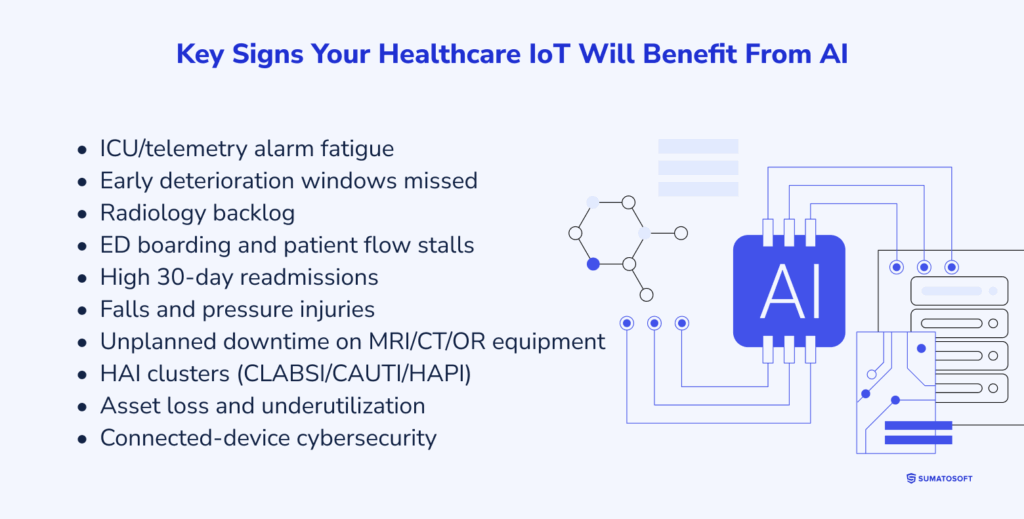
- ICU/telemetry alarm fatigue – false alerts drown staff; true deterioration still slips through. You already stream ECG/SpO₂/BP – use AI to denoise and rank risk in real time;
- early deterioration windows missed – sepsis, AKI, respiratory failure. You have continuous vitals + labs; AI can surface risk hours earlier for faster escalation;
- radiology backlog – CT/MRI/portable X-ray queues grow; AI triage flags critical studies (ICH, PE, pneumothorax) for first read;
- ED boarding and patient flow stalls – door-to-triage and bed assignment lag; AI on IoT + EHR signals predicts admits/discharges and prioritizes transport/turnover;
- high 30-day readmissions (HF/COPD/post-op) – RPM devices stream vitals/weight/SpO₂; AI detects relapse patterns and triggers earlier outreach;
- falls and pressure injuries – persist despite rounding. Smart beds/room sensors exist; AI fuses movement, bed-exit, and vitals to alert before an event;
- unplanned downtime on MRI/CT/OR equipment – device telemetry is available; AI predicts failures to protect schedules and revenue;
- HAI clusters (CLABSI/CAUTI/HAPI) – creep up silently. Device usage + hygiene sensor data can reveal risky patterns before rates spike;
- asset loss and underutilization – pumps, monitors, wheelchairs go missing. RTLS beacons stream location; AI optimizes fleet availability;
- connected-device cybersecurity – currently reactive. Network/behavior baselines enable AI to flag anomalous traffic and firmware behavior fast.
B) When AI Is Overkill (For Now)
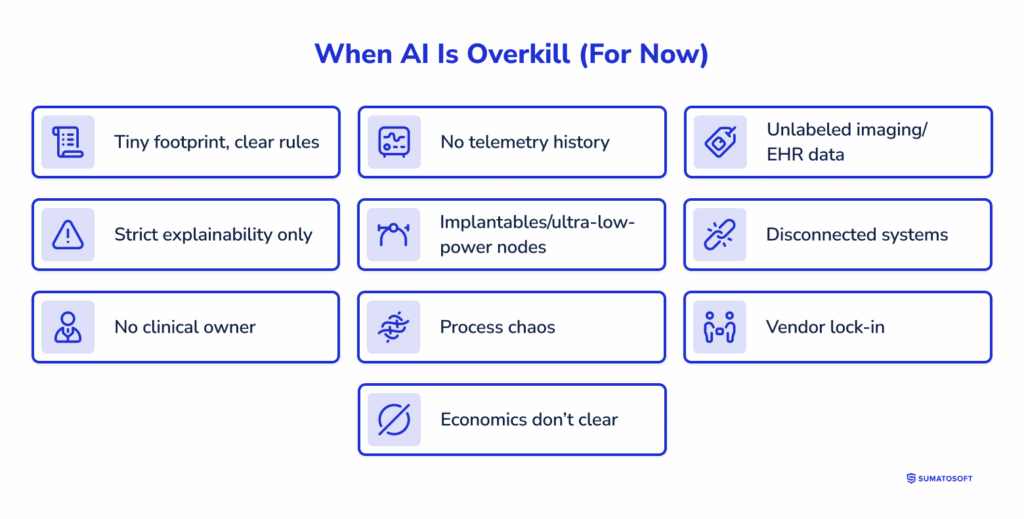
- tiny footprint, clear rules – small clinic or single ward; few devices; thresholds already work; events are rare;
- no telemetry history – weeks not months of vitals, waveforms, or device logs; no outcomes (RRT, codes, readmissions) to learn from;
- unlabeled imaging/EHR data – studies and notes lack ground truth; curation would cost more than the pilot;
- strict explainability only – workflows that legally require transparent logic (e.g., dosing protocols); black-box models won’t pass;
- implantables/ultra-low-power nodes – hardware can’t host even tiny models without hurting safety or battery;
- disconnected systems – no path to write back to EHR/PACS or route alerts to nurse call/secure messaging; insights won’t reach clinicians;
- no clinical owner – no named nurse/physician leader to act on alerts and change practice;
- process chaos – rounding, escalation, and triage vary by shift; standardize first, then optimize;
- vendor lock-in – monitors/pumps don’t expose APIs; data is a walled garden;
- economics don’t clear – low volume or low stakes; a rule/report gives most of the benefit.
C) Run a 1-Week Opportunity Scan (Fast Path) – Healthcare
Day 0 – Frame the pains (90 min)
CMIO/clinician lead, nurse manager, radiology/ED/ICU rep, biomed/IT, privacy/compliance. List top pains: alarm fatigue, missed deterioration (sepsis/AKI/resp), imaging delays, ED boarding, falls/pressure injuries, readmissions, device downtime. For each – define the win in plain words (fewer false alarms, faster reads, earlier escalation).
Days 1-2 – Data + integration check.
- signals – vitals/waveforms (ECG, SpO₂, BP, RR), labs, meds, notes; RPM streams; pump/vent logs; RTLS. History length, sample rates, gaps;
- labels/outcomes – rapid responses, codes, ICU transfers, sepsis flags, falls, readmissions, imaging findings;
- pipelines – EHR (HL7/FHIR), PACS/VNA, monitoring gateways, nurse call/secure chat;
- guardrails – HIPAA, audit trail, model explainability needs, bedside validation plan.
Day 3 – Feasibility + sizing.
Rules vs ML/DL. Edge vs cloud vs hybrid. Clinical validation path (prospective shadowing, silent mode). FDA implications if controlling a device. Rough effort vs. expected payoff; kill candidates with missing data/owner or blocked integrations.
Day 4 – Pick one.
Choose the highest-leverage, feasible case with a named clinical owner and unit to pilot (e.g., ICU, step-down, ED, radiology).
Day 5 – One-pager (decision doc).
Problem & current baseline; target change (e.g., fewer alarms, shorter TAT, earlier sepsis escalation); data plan (sources, history, labeling); model approach; deployment (edge/cloud); EHR/PACS/alert routing; governance & risks; timeline and checkpoints.
End of week – Output: a scoped, defensible pilot plan clinicians can act on, with data paths, owners, and a clear first unit.
AIoT suitability self-assessment
Use this AIoT Suitability Self-Assessment to quickly gauge whether your organization is ready for an AIoT pilot. Download the checklist to score your current state and identify gaps before investing.
KPI Framework in Healthcare
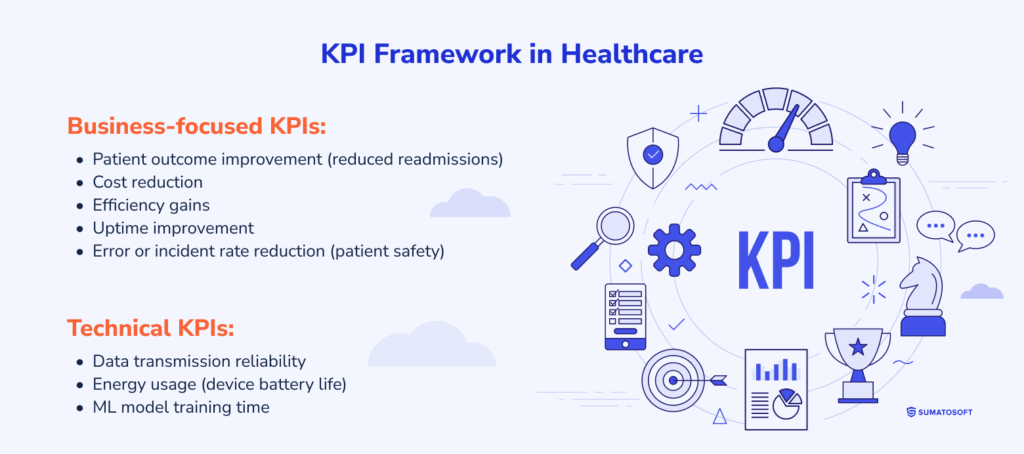
AIoT projects in healthcare must be judged by outcomes, not by technology. KPIs provide that anchor: clear measures that show whether patient care and financial performance have actually improved. In this section, we outline which metrics to track for typical AIoT cases in healthcare, how to establish baselines, and how to monitor progress in a way that matters both to clinicians and administrators.
If you want to know more about the cost of IoT app development, we encourage you to read our article “How Far Can $50k Take You in IoT App Development?”
Business-focused KPIs:
- patient outcome improvement (reduced readmissions) – tracks better health results, e.g., fewer 30-day hospital readmissions; AI-driven remote monitoring can flag complications early, avoiding ~$16k per readmission;
- cost reduction – measures lower costs from fewer redundant tests, shorter hospital stays, and reduced labor; e.g., automated vitals monitoring frees nurse time and cuts overtime;
- efficiency gains – monitors throughput gains such as faster imaging workflows or reduced patient wait times; AI triage can process ER cases minutes faster, improving bed turnover;
- uptime improvement – tracks availability of critical devices; predictive maintenance on MRI machines avoids costly rescheduling and lost billing hours;
- error or incident rate reduction (patient safety) – measures fewer diagnostic or medication errors; AI prescription checks catch harmful drug interactions before dispensing.
Technical KPIs:
- data transmission reliability – ensures wearable or bedside devices deliver over 98% of readings; e.g., heart monitors streaming uninterrupted during ICU stays;
- energy usage (device battery life) – tracks battery longevity; extending wearable ECG monitors from 12 to 24 hours reduces swap-outs and missed data;
- ML model training time – measures how fast models retrain; e.g., updating sepsis risk models overnight to reflect new hospital data.
Calculating Cost Vs. Benefit (With an Example)
Next, let’s move to the calculation part. Our goal here is to turn an AIoT idea into cash flows your CFO will sign off on. Below is a healthcare-specific template and a worked example you can reuse. It adapts the generic math from the source doc to hospital realities.
Step 1: Define the variables
| Metric | Symbol | Unit | Inputs (with units) | Financial benefit (formula) |
|---|---|---|---|---|
| Excess bed-days saved | BD | days/year | Cbed = cost per bed-day ($/day) | |
| 30-day readmissions avoided | R30 | cases/year |
| |
| Clinician time saved (nursing, RT, radiology) | hours/year | = loaded hourly wage ($/hour) | ||
| Imaging throughput uplift | ΔReads | reads/year | = margin per read ($/read) | |
| Critical device uptime (MRI/CT/OR) | hours/year | downtime reduction rate (%); revenue per hour ($/hour) | ||
| Cloud/bandwidth saved (edge filtering) | B | $/year (spend) | = reduction rate (%) | |
| Confidence factor after pilot | α | 0–1 (factor) | – |
|
| Recurring opex | O | $/year | – | |
| One-time costs | K | $ (one-time) | – |
Step 2: Write down core equations
Annual benefits (risk-adjusted):
Annual net cash inflow:
Payback (years):
NPV over T years at discount r:
(If you expect drift, use year-specific Nett.)
Step 3: Perform Calculations
Our working example: radiology AI triage in a mid-size U.S. hospital.
Scope:
- AI triage for CT/X-ray + edge filtering of images;
- goal = free radiologist time, cut cloud egress, add reads.
Inputs (one year):
- Radiologist time saved: 145 work-days ≈ 1,160 hours (published case figure). Loaded cost Wrad = $180/h => Hrad·Wrad = $208,800.
- Cloud/bandwidth spend: B = $120,000/yr; reduction rb = 30% => $36,000.
- Extra billable reads from freed capacity: ΔReads = 1,500; margin $60/read => $90,000.
- Confidence factor after pilot: α = 0.7.
- Recurring opex: O = $120,000/yr (licenses + MLOps + support).
- One-time costs: K = $300,000 (integration, rollout, labeling).
Calculations:
- Gross benefits: $208,800 + 36,000 + 90,000 = $334,800.
- Risk-adjusted: Benefits = 0.7 × 334,800 = $234,360.
- Annual net: Net₁ = 234,360 − 120,000 = $114,360.
- Payback: 300,000 / 114,360 ≈ 2.62 years.
- NPV (T=4, r=10%): ≈ −300,000 + 114,360 × (0.909+0.826+0.751+0.683)
= −300,000 + 114,360 × 3.169 ≈ +$62,000 (positive).
Notes: the 145-day time-savings reference and high ROI of radiology triage come from published hospital examples in the source doc; plug your own wage rates, margins, and vendor quotes.
How to Use It
- Swap radiology for sepsis early-warning: use BD (ICU and ward bed-days saved) and R30 for readmissions avoided at Creadm ≈ $16k per case.
- If device uptime is the driver (e.g., MRI), emphasize Ddev, rd, and Crev.
- Set α to 0.6-0.8 right after pilot; raise it as evidence grows (prospective validation, silent mode, then live).
What’s Next?
Pick one clinical use case and one unit (e.g., ICU alarm denoising, sepsis early warning, or radiology triage), assign a clinical owner, and map data sources (bedside monitors, labs, imaging, RPM) with integrations into EHR (FHIR/HL7), PACS (DICOM), and nurse-call/secure messaging.
Run a short silent-mode under HIPAA with audit trails, calibrate thresholds by unit/diagnosis, and confirm edge vs. cloud plus failover and a clear override path. Then launch a 30-day live pilot in that unit with daily safety checks and a rollback plan, measuring a few simple outcomes (alarm burden, turnaround time, bed-days).
Wrap with a brief readout that translates clinical impact and time saved into dollars for CFO approval and a scale plan.
If you plan to develop your own AIoT healthcare system, we encourage you to reach out to us at SumatoSoft. We specialize in IoT development.
How We Can Help
Build healthcare software that clinicians trust and regulators approve. SumatoSoft is an ISO-certified team (ISO 27001, ISO 9001) delivering AI- and IoT-enabled solutions for providers, digital-health startups, and device manufacturers – with security and compliance from day one.
What we deliver:
- for healthcare providers – we develop and implement EMR/EHR, practice management, lab management, asset tracking, remote patient monitoring, and population health management solutions;
- for digital-health startups – we provide expertise to create innovative telehealth systems, wellness tech solutions, and software for diagnostic and healthcare monitoring devices;
- for device manufacturers – we empower hospital-grade and consumer devices with robust healthcare device management solutions across web and mobile platforms, enhanced by AI-powered analytics.
How we work:
- consulting & R&D – architecture, interoperability (HL7/FHIR), threat modeling, and guidance on HIPAA/FDA/GDPR/HITECH/SSAE;
- custom healthcare software development – frontend, backend, and mobile (mHealth) with robust integrations (EHR, LIS/RIS/PACS, payment/billing);
- custom healthcare AIoT development – IoT-powered healthcare solutions backed by the capabilities of Artificial Intelligence.
- AI & analytics – predictive models, streaming/edge pipelines, and dashboards that support clinical decisions and operations.
Why SumatoSoft
- compliance first – HIPAA, GDPR, FDA, HITECH, FHIR/HL7; security aligned with OWASP, PCI, FISMA;
- transparent delivery – Agile sprints, clear estimates, regular demos, and measurable KPIs tied to outcomes;
- top IoT development company – awarded by Clutch, goodfirms, and techreviewer.
Book a free consultation, and we will provide a discovery session to assess the cost of your project development.
Let’s start
If you have any questions, email us info@sumatosoft.com




